Breathing lifesavers: How Respiratory Therapists are firefighters of hospitals
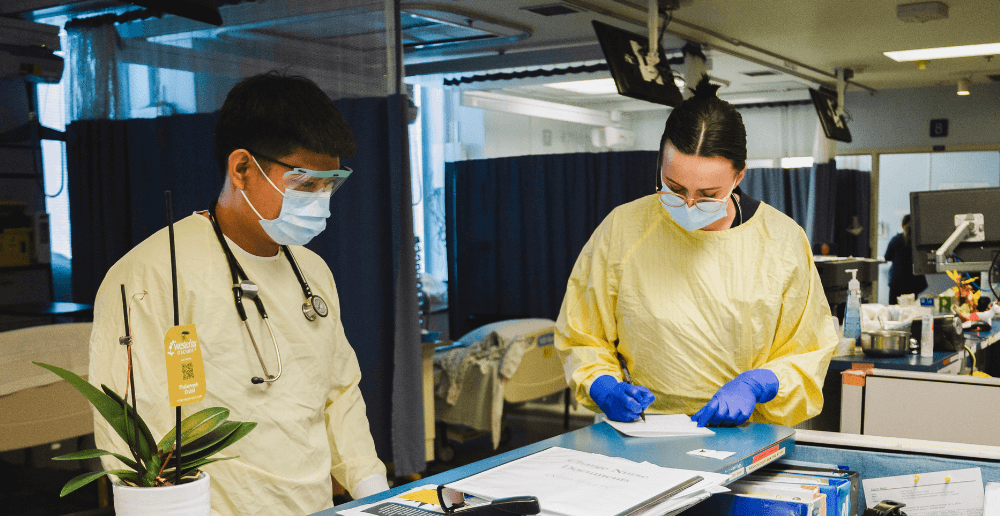
Follow a day in the life of Laura Wall, RT at Grace Hospital

Winnipeg Regional Health Authority
Published Tuesday, October 24, 2023
Respiratory Therapist Laura Wall likens her profession to being a firefighter; always responding to emergencies as quickly as possible, as soon as the intercom page comes. In honour of national Respiratory Therapy week, Wall shared some insights into her challenging and deeply rewarding role - from helping patients adapt to life with home oxygen to participating in life-saving code blues. Laura also reveals the poignant side of her job, the moments that tug at her heartstrings when - despite her best efforts - some patients don't make it. Learn how she copes with these losses and continues to make a profound impact on the lives of those she cares for.
Note: this conversation is a transcript that has been edited for clarity and length.
How would you describe your job to someone not familiar with respiratory therapy?
I describe myself as kind of like the firefighter of the hospital. As soon as the code blue bells go, we are responding to any emergency that happens within the hospital. We do have some patients that we follow, like the patients in the ICU. We're following them every day, all day, all night. But we're also putting out fires as they come up. So no one day looks the same for us.
Did you always want to be a respiratory therapist?
My mom has a book [from] every grade [where] I would write different answers to questions. And in grade two, it first asked me what I wanted to be when I grew up. And I said, ‘I want to help people to feel better.' So in elementary school, I wrote like, nurse, doctor - because that was kind of all I knew. And then in high school, my auntie was a physio here [at Grace], so I did Take Your Kid to Work day here and was obsessed with physiotherapy [and] occupational therapy. When I was looking up physio and occupational therapy schools, I came across respiratory therapy and I had every single prerequisite. So I was like, oh, I'll just apply - and then I got in.
What aspects of your job do you enjoy the most?
I really enjoy the moments that I can directly see my impact on people. So I do eight hour shifts where I'm working with home oxygen and on those shifts, I have the time to sit down with patients and their family and help them to understand what life is going to look like for them once they go home on oxygen. And kind of helping them to adapt to that reality. I drop off this booklet that says, ‘you're going home on oxygen,' and I see the anxiety builds, but then I get to sit with them and talk it through. I can spend 20 or 30 minutes with them and just see them calm down. That's really rewarding.
The more exciting things are when you're going to a code blue, or a moment where you don't know if the patient is going to make it or not, and you're doing everything that you can - and they pull through.
And then the best moments are often when a patient is in our ICU. We've worked on them for days, or weeks, or however long it's been, and they're finally ready to come off the ventilator. That's us pulling [out] the breathing tube and encouraging them to take their first breath off of the machine and use their voice again for the first time in days or weeks. And sometimes the family is there, and it's just a really nice moment.
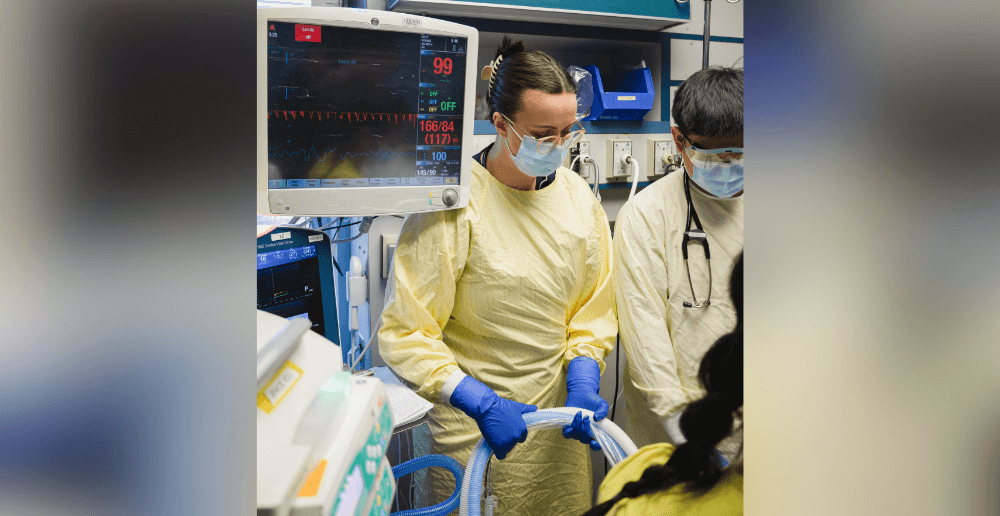
What does coming off the ventilator look like?
So there's a big kind of balloon in your airway. I'm holding [the breathing tube], I deflate the balloon, and I turn off the ventilator. I get them to take a big breath in, and then I just pull it out and I'm saying ‘cough for me'. And I'm trying to suction up anything that they're coughing up. Usually we put them on some oxygen, so they're not just breathing room air. Then it's usually touch [and] go for a little bit. You don't really know necessarily, the person that you think is going to be totally fine might need [the ventilator] to be put back in.
What are the most challenging parts of your job?
So the same as the most exciting parts being when it's touch and go and . . . they pull through, there's a lot of times that they don't. And that can be really hard because often those are the moments - when they crash - there's no family there. So we are there at the end of that person's life. That can be really hard. When families are there, it's equally, if not more upsetting. When you're in the ICU, you're on [medication] keeping you alive. But that's not very [noticeable] for the family. The visual thing is the ginormous breathing machine and the tube that's pushing air in and out. So to be the person that's going in there to take that out . . . that's like the most visual, symbolic thing to the family. I [will] go in [the room] and say, I'm so sorry for your loss . . . this is what I'm about to do.
How do you cope with the losses?
There's definitely ones that hit you more than others, like patients that you've been following on the ward, and then they end up coming to the ICU and they end up getting intubated. So you're caring for them over the course of two, three, four weeks, and you get to know their family a little bit more.Ultimately, they have to decide to withdraw [the ventilator]. That still gets me. It can be pretty heavy.
I had one patient on the ward that I was following for about a week, and she was on the maximum amount of oxygen that we can do up there. She was 99-years-old, so it was definitely her time. But she would talk with me, because no family was ever there. So I would go up in my free time and I would just chat with her for like 20 or 30 minutes some days. And [one day] I went in and she said, ‘Laura, today is the day that I'm going to die.' And I was like, whoa, you know that? She's like, yeah, I woke up and it's my time today.
She died a half an hour after I left. She talked to me so much, and she told me so many things about her life . . . she was just the sweetest little woman. I waited for her obituary to come out, and I read it. So that [loss] really got me. But they can't hit you like that every single time.
Describe a time when you were coming to work, or you were leaving work, and you felt affirmed in your decision to pursue a career as an RT.
Recently, I was off for nine days. I didn't miss it, but I was excited to come back. A lot of my friends . . . we're all kind of starting our careers, we're all in our mid 20s, and a lot of people dread going to work, and I don't. I feel very fortunate for that. I never know what I'm going to get up to. So walking home every day, I always feel like I have a story to go home with, to tell, or to journal about. It's a pretty adrenaline filled job, which I like. In our downtime, like in the [break] room, I'll be reading my book, I'll be doing my colouring. When I'm not needed, I'm not needed. But then all of a sudden the bell rings, and we're off.
Laura Wall is a respiratory therapist working at Grace Hospital in the Winnipeg health region. This ‘day in the life' story is part of a series of first-person articles to recognize the unique and specialized skills and abilities of allied health professionals during Allied Health Professionals Week from November 5-12, 2023.